By: Ranier Simons, ADAP Blog Guest Contributor
Many members of society are adversely affected by inequalities stemming from diverse circumstances and socio-economic realities. Disparities in public health result from those inequalities. Policy is one avenue for improving the health of those in need. One policy response by Congress was the creation of the 340B Drug Pricing Program as part of the bipartisan Veterans Healthcare Act of 1992.[1] The 340B program allows qualifying safety-net providers and qualifying hospitals, otherwise known as covered entities, to purchase prescription drugs at significantly discounted prices from manufacturers and re-invest those dollars in expanding access to care and treatment. A growing chorus is concerned that the legislative intent of the program is being obfuscated by large hospital systems and mega service providers.
 |
| Photo Source: USA Today |
These covered entities serve low-income and vulnerable populations who are uninsured, on Medicaid or Medicare. The savings generated from the program are used to offer patients free or discounted drugs and provide many other services that meet the healthcare needs of the communities these entities serve.[1] Other services include prevention-focused primary care, mental healthcare, and substance abuse treatment. What started out as a good idea has evolved into a system where inefficiencies and abuses have corrupted 340B’s intent and harmed some patients. As a result, on a federal and state level, numerous pieces of 340B reform legislation have been introduced to stop abuses, protect patients, and overall ensure the program operates as intended.
One issue is the sheer number of covered entities taking advantage of the 340B discount pricing.[2] At the program's advent, safety-net hospitals, outpatient clinics, and community health centers were the first entities allowed to participate. Later, Congress expanded eligibility to add children’s hospitals, outpatient cancer center hospitals, rural referral centers, sole community hospitals, and critical access hospitals. Covered entities are supposed to serve large numbers of vulnerable community members by providing charity care and passing on savings. However, the lack of robust oversight and ambiguity in the 340B legislative language has allowed some entities to take advantage of the program. Some entities abuse the program by using the savings for profit instead of passing them on directly to patients or using them for services to serve them. Some entities participate in the program when they should not be qualified. Some larger hospitals do this by manipulating their business structures by acquiring smaller entities that qualify in the true spirit of the program.
Another significant issue is bad faith actions from some covered entities who are using 340B rebates to fund exuberant executive compensation, which is entirely made more egregious by the hospital systems simultaneously cutting their charity care for indigent patients.[3]
A notable piece of legislation recently introduced in Congress to affect 340B reform is a discussion draft bill entitled the ‘SUSTAIN 340B Act’ - which stands for ‘Supporting Underserved and Strengthening Transparency, Accountability, and Integrity Now’.[4] It was introduced by U.S. Senators John Thune (R-S.D.), Debbie Stabenow (D-Mich.), Shelley Moore Capito (R-W.Va.), Tammy Baldwin (D-Wis.), Jerry Moran (R-Kan.), and Ben Cardin (D-Md.), all members of the Senate 340B bipartisan working group. This bill is a comprehensive attempt at reform targeting many of the current weaknesses of the 340B program. It addresses multiple areas, such as transparency, contract pharmacy operations, program integrity, and accountability.
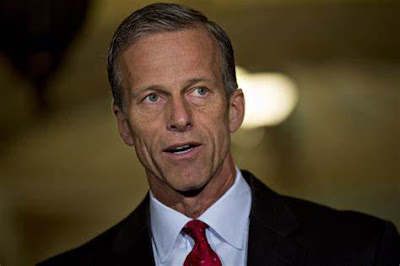 |
| Sen. John Thune | Photo Source: TIME |
In one vein of accountability, this bill amends the current 340B legislation by defining parameters for what can be considered ‘child sites’.[4] Many covered entities operate more than one physical location. An example is a non-profit hospital that may have multiple clinics or service centers outside the main hospital where all entities are partaking of the 340B discount. This bill explicitly defines the operating relationships required to be considered a qualifying child site. This is necessary because many entities are improperly spreading their 340B privilege across outlets under their umbrella.
Another accountability measure defined by the SUSTAIN 340B Act relates to reporting. Concerning patient and community benefits, the bill requires covered entities to show their proverbial ‘receipts’ and thus bringing some much-needed transparency to the program. The legislative verbiage mandates the reporting include data such as the financial demographics of covered entities served populations, specifics on how the 340B prescriptions utilized by patients improved their health, explanations of policies covered entities use to promote access and adherence to prescribed medication, and even detailed reporting of how the discounts received from the program are used.[4]
The legislation, in part, reads: “We believe that requiring covered entities to report detailed information regarding their program savings, policies, patient and prescription information, and then enabling that information to be publicly available by the Secretary will help ensure all stakeholders have trust and confidence that the program is being used as intended.”[4]
A more contentious part of the bill targets drug manufacturers. The bill specifically defines things that drug manufacturers cannot do. An example is where it explicitly states a drug manufacturer cannot impose a restriction on a covered entity as a condition to receive a discount, such as “…requiring the submission of claims data directly to the manufacturer out of submissions to the entity receiving the contract to maintain the clearinghouse under section 1150D of the Social Security Act.”[4] Most importantly, the bill defines prohibited activity, legal remedies, and monetary penalties that can be assessed if drug manufacturers break the rules.
The SUSTAIN Act also aims to enhance program integrity by implementing stronger guidelines for government audits of covered entities, preventing duplicate discounts by bad actors gaming the system between the 340B program and Medicaid, and reigning in health plans and pharmacy benefit managers attempts to restrict access to drugs in the 340B program.[4]
Dusty Garner, a long-time survivor of HIV and member of the ADAP Advocacy 340B Patient Advisory Group, passionately summarized: "Listen, it is about damn time Congress opened the books on this $54 Billion program and asked the corporate healthcare providers who are benefiting the most from it to do the same with their ledgers. Too many patients are drowning in medical debt, yet they're residing in areas with so-called nonprofit hospitals supposedly best suited for expanded access under the 340B Program. Where is all of this money going, cause we know too much of these 340B rebates aren't helping the patients who most need it."
-FINAL.jpg) |
| Photo Source: CANN |
Another less notable piece of legislation introduced was the ‘340B Pharmaceutical Access To Invest in Essential, Needed Treatments & Support Act of 2024’, known as the 340 B PATIENTS Act.[5] It was introduced by Rep. Doris Matsui (D-Calif.), a known drug industry antagonist and a favorite of the American Hospital Association. Despite the legislation's short title, it appears to be more concerned with providers than patients. The 340B PATIENTS Act is not as comprehensive as the SUSTAIN Act. Its specific focus is to make amendments concerning contract pharmacy dealings and drug manufacturer enhanced reporting requirements. One section of the bill adds amended language to clarify that drug manufacturers are required to “offer 340B pricing for drugs purchased by a covered entity regardless of the manner or location in which the drug is dispensed, and section 340B prohibits drug manufacturers from placing conditions on the ability of covered entities to purchase and use 340B drugs, regardless of the manner or location in which they are dispensed.”[5]
Thomas Johnson, Executive Director of ASAP 340B, expressed sentiments concerning the 340B PATIENTS Act. He states, "While we welcome efforts to address 340B contract pharmacy arrangements, the 340B program needs comprehensive reforms that will restore its integrity and accountability and, most importantly, ensure underserved communities are benefiting. ASAP 340B was formed because nearly all stakeholders involved in the 340B program have grave concerns about its ability to serve the nation's safety net as was originally intended 30 years ago. Community Health Centers, patient, provider and consumer advocates, and leaders from the biopharmaceutical industry are at the table together, working with Congress on solutions that will go further to address the flaws in the 340B program currently putting America's safety net at risk."
 |
| Photo Source: ASAP 340B |
The 340B program is a lifeline for covered entities and the communities they serve. Fighting to legislate its survival is imperative to improve the health and lives of those truly in need of its benefits. In a joint statement to the U.S. Senate Bipartisan 340B Working Group in response to a Request for Information, ADAP Advocacy and Community Access National Network perfectly described the dire need for reform. They explain: “When originally drafted, Congress did not include extensive parameters to govern the entities. This means that the statute is silent on many critical program requirements that are necessary for it to function correctly today, ensuring that patients, and not hospital networks, are seeing the benefit of discounted medicines. But it is now more than 20+ years later, and difficult to argue about what occurred then as compared to now. The challenge and the opportunity are to focus on what Congress wants the program to be today, who it should serve, what healthcare providers should be qualified as “covered entities,” etc.[6]
The current toxic political environment on Capitol Hill, which is exacerbated by the continued dysfunction in the House of Representatives, makes it highly unlikely anything gets done in Congress other than funding the government. But the introduction of 340B-specific legislation does demonstrate that the growing calls for reform of the 340B Program are finally being heard. The simple truth of the matter is the more patients learn about how the 340B Program could be better serving them rather than lining the pockets of corporate healthcare providers, they’re left asking: “340B: What about me?” Congress appears to be listening.
[1] HRSA. Sec. 340B Public Health Service Act. Retrieved from https://www.hrsa.gov/sites/default/files/hrsa/rural-health/phs-act-section-340b.pdf
[2] The Commonwealth Fund. (2022, September 8). The Federal 340B Drug Pricing Program: What It is, and why it’s facing legal challenges. Retrieved from https://www.commonwealthfund.org/publications/explainer/2022/sep/federal-340b-drug-pricing-program-what-it-is-why-its-facing-legal-challenges#:~:text=In%202015%2C%20the%20U.S.%20Government,left%20largely%20to%20police%20themselves.
[3] Hopkins, Marcus J.. (2023, November 2). 340B Covered Entities’ Revenue Witnessed Huge Executive Compensation Increases, Alarming Charity Care Decreases. The ADAP Blog Retrieved from https://adapadvocacyassociation.blogspot.com/2023/11/340b-covered-entities-revenue-witnessed.html
[4].Thune, J., Stabenow, D., Moore, S., Baldwin, T., Moran, J., Cardin, B. (2024). SUSTAIN Act. Retrieved from https://www.thune.senate.gov/public/_cache/files/c3a678e3-12a5-4175-8a80-9246b76576ec/75E01A8968B679E3525395E2BB0CE7DB.ss340b-act-discussion-draft-.pdf
[5] Matsui, D. (2024, March 12). 340B PATIENTS Act. Retrieved from https://matsui.house.gov/sites/evo-subsites/matsui.house.gov/files/evo-media-document/MATSUI_022_xml_final.pdf
[6] ADAP Advocacy, Community Access National Network. (2023, July 23). Joint Statement. Retrieved from https://www.adapadvocacy.org/pdf-docs/2023_ADAP_CANN_Public_Comment_Senate_RFI_340B_07-24-23.pdf
Disclaimer: Guest blogs do not necessarily reflect the views of the ADAP Advocacy Association, but rather they provide a neutral platform whereby the author serves to promote open, honest discussion about public health-related issues and updates.














